Find your answers to common questions about Alpha-Mannosidosis.
Questions are organized by topic to make searching easier.
Click over each question to find the answer you need.
Frequently asked questions about Alpha-Mannosidosis
Alpha-Mannosidosis is a rare hereditary disease that can cause children and adults to suffer from skeletal deformities, coarse facial features, hearing loss, mental retardation, problems with the immune system, psychiatric disorders, and behavioural problems.1
When the gene that provides instructions for making the Alpha-Mannosidase does not function properly, the enzyme is not produced correctly, causing Alpha-Mannosidosis.2
This enzyme works in the lysosomes, which are compartments that digest and recycle materials in the cell. Within lysosomes, the enzyme helps break down long chains of sugar molecules (oligosaccharides). Oligosaccharides are used in the building of bones, cartilage, skin, tendons and many other tissues in the body.2,3
In people with Alpha-Mannosidosis, partially broken down sugars remain stored in the body and build up over time. This causes increasing damage to the cells.2 Babies may show little sign of the disease but as more and more cells become damaged by accumulation of oligosaccharides, symptoms start to appear.3
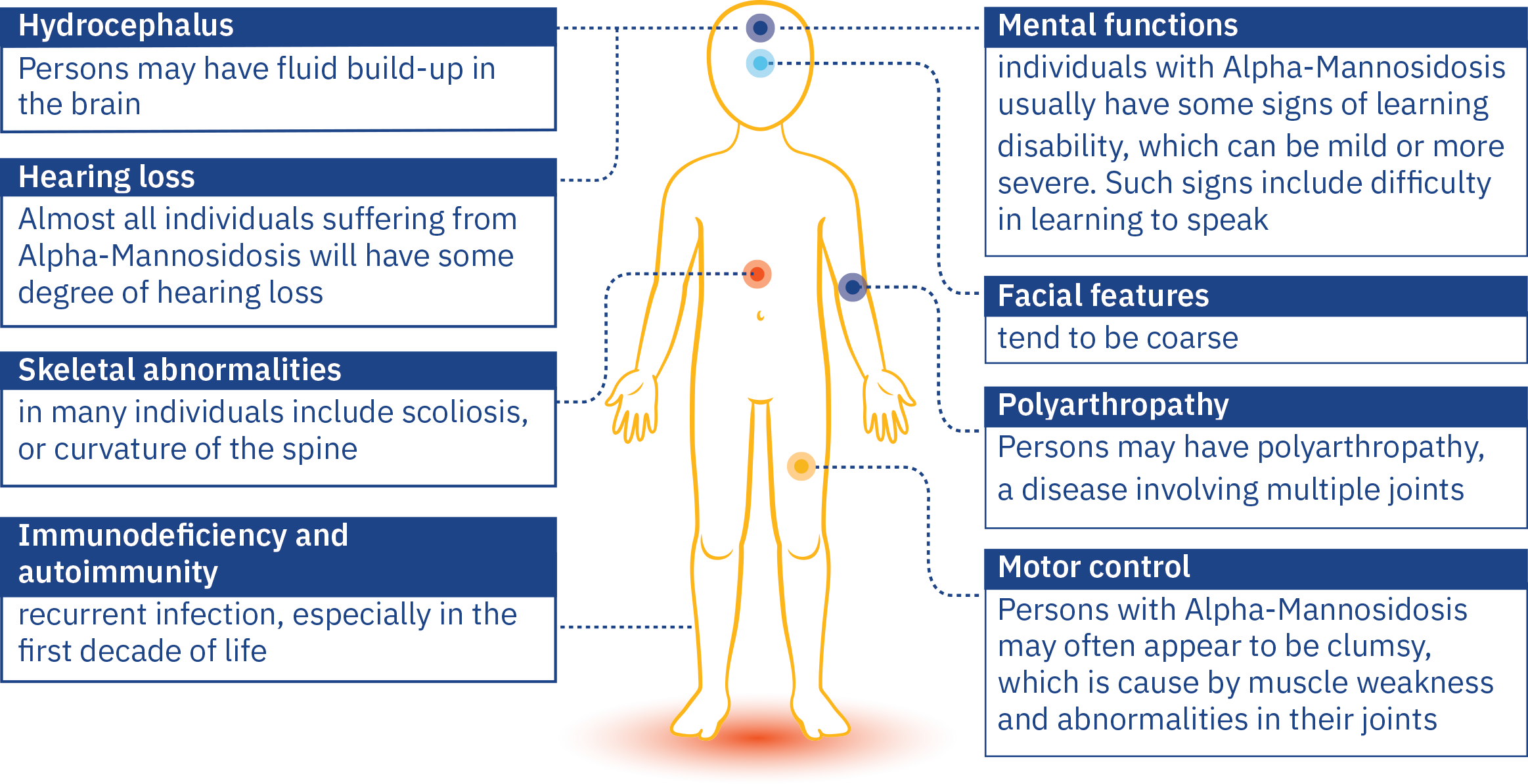
The symptoms of Alpha-Mannosidosis, like other related disorders can be very variable.1
It is a progressive disease, which shows itself in a variety of ways over a period of time.4
Because it has such a wide range of symptoms, and as each individual will experience their own unique pattern of symptoms, diagnosis can take a long time.4
During the first decade of life, a child with the condition may have frequent infections, hearing problems, distinctive facial features and developmental delay.1,5
Parents might notice that their child may have some muscle weakness.4 There may be an unusual feature such as a club foot, a large head, unusual appearance, maybe a bent back. A child may have attention problems and struggle with hearing.3,4 One symptom could be a one-off, but the combination of symptoms at the same time is no coincidence. Consider all the symptoms, and seek referral to a metabolic specialist by asking your family doctor to refer you.
In their 20s and 30s, an adult may experience bone problems and difficulties with movement, such as joint problems, swelling, an unsteady gait and muscle weakness. Ultimately, patients may become dependent on a wheelchair, as they can no longer walk on their own.1
There may be behavioural or psychiatric problems, which can present as episodes of confusion, sometimes with anxiety, depression or hallucinations.1
Independent living will be difficult, and Alpha Mannosidosis patients may become socially isolated.1,6 The long-term forecast for the condition is poor.1
Three clinical subtypes have been proposed:1
Type 1
MILD FORM
Recognized after ten years of age, with very slow progression, and absence of skeletal abnormalities.
Type 2
MODERATE FORM
Recognized before ten years of age, with presence of skeletal abnormalities, slow progression, and development of ataxia at age 20-30.
Type 3
SEVERE FORM
Immediately recognized with skeletal abnormalities and obvious progression leading to early death from progressive central nervous system involvement or myopathy.
However, given the variety of mutations that have been documented, the broad range and severity of symptoms, and no link of particular mutations to clinical subtype, the disease is considered clinically as a continuum from mild to severe.5,6
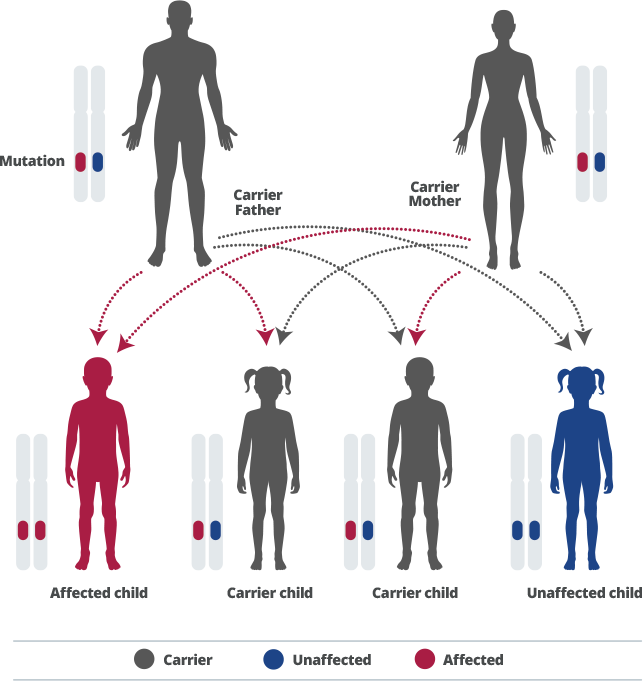
Alpha-Mannosidosis is inherited, meaning it runs in families.1
Genes are inherited from our parents. We inherit a copy of each gene from each parent. Some genes we inherit are “recessive”, which means that both copies of that gene need to be inherited for it to have any effect on our development.7
Alpha-Mannosidosis is caused by a recessive gene.1 Each pregnancy of a couple in which both partners are heterozygous for a disease-causing mutation of the MAN2B1 gene has a 25% chance of having an affected child, a 50% chance of having an unaffected child who is a carrier, and a 25% chance of having an unaffected child who is not a carrier.8
As the disease is so rare, the chance of having a partner who is another carrier is slight, unless the individuals are of the same family. If a couple already has a child with the condition, genetic counselling is recommended, to understand the chances of the disease also occurring in future offspring.3
The prevalence of Alpha-Mannosidosis is not known exactly. However, a number of reports from different countries estimate that it occurs in approximately one in every million babies born worldwide.5
Your doctor can use a number of very simple tests to diagnose Alpha-Mannosidosis, including:
- A physical check-up with medical history.1 If a diagnosis of Alpha-Mannosidosis is suspected, your doctor may take urine and blood samples to rule out other clinical conditions and confirm a diagnosis.
- Urine sample.1 This will measure oligosaccharide levels in urine. High levels will be suggestive of Alpha Mannosidosis.
- Blood sample.1 A small sample of blood is taken to measure the presence of mannosidase enzyme in blood cells. This can be used to confirm a diagnosis.
- Genetic testing.1 A diagnosis of Alpha-Mannosidosis can also be confirmed through genetic testing, which can detect the mutation in the gene that causes the disorder.
There’s a supportive community out there that’s eager to provide information sources, understanding and advice. A host of organisations and support groups is just a few clicks away.
Patient organisations:
ISMRD is the international support group for Alpha-Mannosidosis.
Lysosomal Diseases New Zealand is the support group for families in New Zealand.
Other MPS groups around the world will also offer support. MetabERN is a network of healthcare providers and patient groups across Europe, providing support for people with inherited metabolic disorders such as Alpha-Mannosidosis.
A diagnosis of Alpha-Mannosidosis can have a considerable emotional impact on patients and caregivers. Access to primary and specialty care and social services needs to be provided, and nutritional and psychological support should be assessed on an ongoing basis.9 Clinical care should be proactive, with doctors planning to limit the consequences of the condition and any complications for patients.1 Joint or other orthopaedic surgery may be considered.1 For more information on management options, please discuss with your doctor.